

The present systematic review was carried out according to the Preferred Reporting Items for Systematic Review (PRISMA) standards. Although the risk of meningitis is the highest within the first week after brain injury, it has been widely documented that meningeal infection might develop after several months, or even years, and a remote mild head trauma might be the only identifiable risk factor in otherwise unexplained cases, especially those recurring over time. Post-traumatic meningitis stricto sensu refers to a meningeal infection causally related to a cranio-cerebral trauma, regardless of temporal proximity therefore, meningitis following neurosurgical procedures (e.g., craniotomy, in-dwelling catheter placement), even those performed because of severe TBI, will not be discussed here. Among several predisposing factors, traumatic brain injury (TBI) is of particular interest, not only owing to its prevalence and its potential intrinsic severity indeed, post-traumatic meningitis is a dreadful condition that presents additional challenges, in terms of both diagnosis and management, when compared with community-acquired cases. The occurrence of meningitis is mostly related to microbial agents, particularly bacteria (so-called pyogenic meningitis), but meningeal involvement may also be secondary to solid/hematological malignancies, autoimmune diseases (including the recently described IgG4-related hypertrophic pachymeningitis), and other causes of aseptic inflammation (e.g., drug-induced).
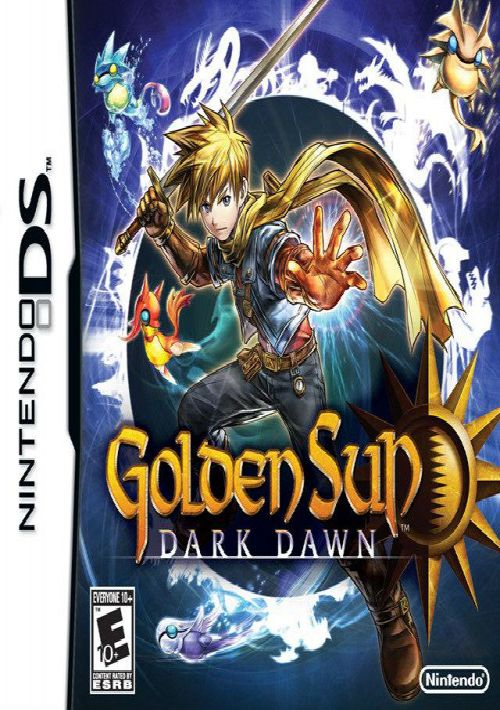
#GOLDEN SUN ROM H UPDATE#
An update on these issues is certainly of interest to focus on possible predictors of survival and useful tools for prompt diagnosis.ĭespite the dramatic decrease in incidence and mortality rates observed over the past decades, especially in high-income countries, meningitis still represents a medical emergency, which requires early diagnosis and prompt treatment in order to avoid death or serious neurological sequelae. On the other hand, radiological exams, especially CT of the brain, could represent an alternative for early diagnosis. On one hand, microbiological exams on cerebrospinal fluid (CSF), which represent the gold standard for the diagnosis, require days to get reliable results.

Among all the detectable clinical signs, the appearance of cranial cerebrospinal fluid (CSF) leakage (manifesting as rhinorrhea or otorrhea) should always arouse suspicion of meningitis. Moreover, these markers increase with a rather long latency, thus not allowing a prompt diagnosis, which could improve patients’ outcome. Diagnosis may be difficult both because clinical signs are nonspecific and blurred and because of the lack of pathognomonic laboratory markers. Post-traumatic meningitis represents a high mortality disease. Studies examining post-traumatic meningitis, paying particular attention to victims of traumatic brain injury, were included.
The PICO (participants, intervention, control, and outcomes) question was as follows: “Is there an association between traumatic brain injury and post-traumatic meningitis?” The present systematic review was carried out according to the Preferred Reporting Items for Systematic Review (PRISMA) standards.
(Mode7)-13.jpg)
Post-traumatic meningitis refers to a meningeal infection causally related to a cranio-cerebral trauma, regardless of temporal proximity. Post-traumatic meningitis is a dreadful condition that presents additional challenges, in terms of both diagnosis and management, when compared with community-acquired cases.


 0 kommentar(er)
0 kommentar(er)
